What is TMJ?
I thought everybody had a stiff neck and
sore shoulders by three in the afternoon!
—a 38-year-old salesman
I can't believe the source of all this
pain is in my mouth.
—a 50-year-old singer
Temporomandibular joint dysfunction syndrome
(TMJ) is the name given to an array of symptoms, the majority
of which are related to muscle spasms. The muscles involved
in the spasms are those which control the movement of the
lower jaw. Because we walk on two legs instead of four, these
muscles also balance the head, neck, and shoulders.
Why do these muscles go into spasm, with disturbing
and sometimes debilitating consequences? The easiest way to
explain the reasons for the dysfunction is to describe the
normal workings of the jaw and the temporomandibular joint.
BONES AND MUSCLES
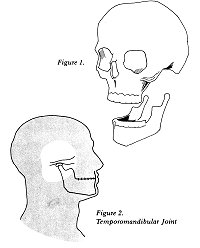
Your upper teeth are connected rigidly to your
skull. Slightly in front of your ears, on your skull, is a
specially shaped bone called the temporal bone. The lower
jaw, which is called the mandible, is a horseshoe-shaped bone;
its free ends rise upward and end in structures called condyles
(see Figure 1) The joint between the temporal bone of the
skull and the condyles of the mandible is called the temporomandibular
joint (see Figure 2).
If you put your fingers in your ears, press
forward, and open. and close your mouth, you can feel the
condyle move. When you open your mouth, only the lower jaw
moves. You can see this for yourself when you look in the
mirror and open and close your mouth.
MOVEMENT IN THE JOINT
Although you have a temporomandibular joint
on each side of your head, the two condyles directly affect
each other's movement. The reason is that the lower jaw rigidly
connects them. When we talk about movement in the joint, we
refer to movement occurring on both sides.
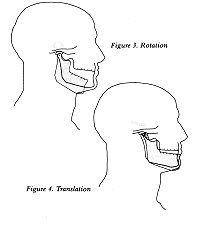
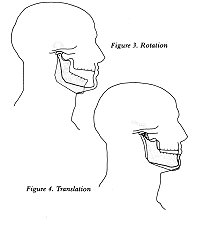
The temporomandibular joint produces two kinds
of movement. It can rotate, making a movement like a door
hinge (see Figure 3). It can also translate, that is, slide
smoothly, much like a ski gliding across the snow (see Figure
4).
The condyle can translate and rotate at the
same time. When you begin to open your mouth, the condyle
rotates for a very short time. After the initial rotation,
it translates forward. Because the condyles are connected
by the jawbone, a side-to-side movement produces motion on
both sides. If you move your jaw to the left, the right condyle
will move down, forward, and in. The condyle on the left will
rotate and move outward. Moving your jaw to the right will
produce the same motions in reverse.
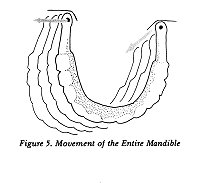
The temporomandibular joint has a protective
cartilage disc between the upper and lower bones. The disc
cushions the bones and prevents them from touching each other.
The joint also has ligaments, which act as wires to limit
the jaw's range of motion. Between the skull and the lower
jaw are groups of paired muscles that control the jaw's movement.
These muscles are called the muscles of mastication.
MUSCLE GROUPS
To give the whole picture, it's necessary to
describe these muscle groups and their location. We speak
of a muscle in the singular, but remember that each of these
has a twin on the other side of the head.
Three pairs of muscles are mainly responsible
for closing the mouth. These are the Temporalis, the Masseter,
and the medial pterygoid (see Figures 6,7,8). To open the
mouth, Mylohyoid and Digastric muscles work through a chain
of other muscles to pull the lower jaw down.
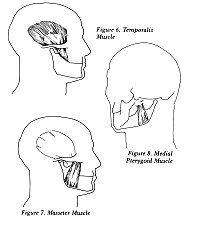
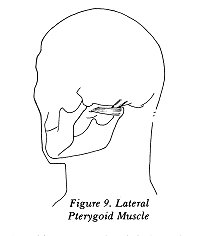
The small Lateral Pterygoids are located deep
within the jaw (see Figure 9). Although they have one name,
they are actually two muscles originating from the same bone
in the skull. One of these muscles connects to the condyle,
and as the muscle contracts it pulls the condyle forward.
Because of the various restricting ligaments, contraction
of the muscle moves the jaw open. The second of the Lateral
Pterygoids is connected to the disc, and its main purpose
is to position the disc when the jaw is closed.
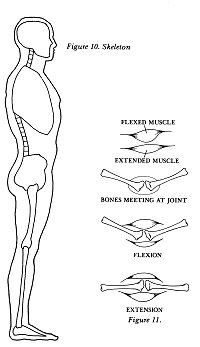
The skull and jaw mechanism is balanced precariously
at the top of the spinal column. The spinal column rests on
the pelvis, which is in turn supported by the legs. At the
upper part of the body, the arms are supported by the rib
cage and shoulder complex (see Figure 10).
The muscles connect bone to bone over joints.
When muscles contract—shorten their length—they
flex the joint. Muscles have no ability to push. They can
only be pulled back to their normal resting length when other
muscles flex the joint in the opposite direction. The muscles
that do this are usually on the other side of the joint (see
Figure 11).
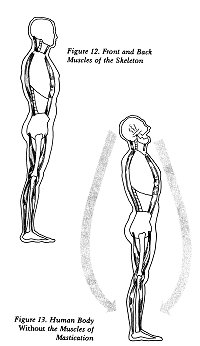
In the front of the body, the muscles extend
from the toes, up the front of the legs, through the pelvis
and abdomen, up to the ribs and shoulders, to the front of
the neck, and then connect to the lower jaw. The muscles in
the back of the body go from the heel through the Achilles
tendon, up the back of the legs, the pelvis, the spinal column,
ribs, shoulders, and finally end up at the base of the neck
on the skull ( see Figure 12).
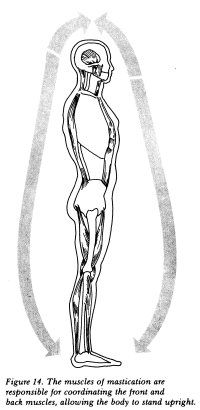
For us to stand upright, the muscles in the
front and the back of the body must be co-ordinated. The muscles
of mastication assume this job because of their location between
the front and back muscles. This co-ordination function is
in addition to their job of opening and closing the jaw. Were
it not for the muscles of mastication, we would walk with
our heads thrown back, our mouths wide open, looking at the
sky (see Figure 13).
CO-ORDINATION
For us to function normally and carry out all
the motions and activities we engage in every day, each of
these muscles must work in a co-ordinated fashion with every
other muscle. If for any reason a muscle is stressed, it affects
all the other muscles in the chain from our toes up through
our jaws and down again to our heels. Because of this interdependency,
the muscles of mastication have a profound effect on our posture
and the ways our bones move (see Figure 14).
Our muscle system, plus the nerves, sensors,
and reflexes that control it, are given a collective name:
the neuromuscular system. Most of the time, the neuromuscular
system works on an unconscious level. We don't think about
the millions of movements we carry out every day. We become
conscious of our movements only when this workhorse system
needs to protect itself.
Like most systems in the body, the neuromuscular
system possesses a marvellous ability to take care of itself,
or at least minimize damage. Consider what happens when you
walk down the street, step off a curb, and twist your ankle.
You may be conscious of pain. Usually you are
able to regain your balance and composure and keep on walking.
But if the twist was severe enough, you may limp. The limp
is the neuromuscular system's way of protecting a potentially
injured component.
The neuromuscular system protects itself by
using muscles that normally have other functions, as well
as changing normal patterns of muscle contraction. We attempt
to avoid further injury by this unconscious mechanism. (Athletes
and dancers often overextend their bodies and play or perform
despite injuries. They sometimes suffer severe consequences
by bypassing nature's protective system.)
The limp is an example of the way muscular activity
in a leg will follow a repeatable pattern. Because of each
muscle's dependence on the whole group, this pattern—in
this case a limp—will create a corresponding change
in movement patterns in all the other muscles interconnected
to it in the chain.
Usually our injuries are slight. The pain of
a twisted ankle is gone in a day or two. But if an injury
is severe and we limp for a long time, then other muscular
problems such as backache are likely to occur.
A SPECIAL JOINT
Muscles are muscles. The muscles of mastication
are no different from any others. However, the temporomandibular
joint is different from all other joints in its ability to
rotate and slide. Even more significant, it has a set of gears
connected to it, and each of its parts is forced to mesh.
The gears are teeth or tooth replacements such as dentures.
You may not think of your teeth as gears, but that's exactly
their function in this mechanism.
The teeth, the structures that surround them,
and the temporomandibular joint contain sensors for the neuromuscular
system. These sensors program the way the jaw moves, similar
to the way a computer program will determine how the computer
functions.
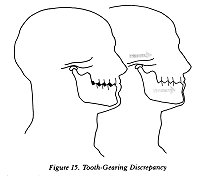
If there is any abnormality, the neuromuscular
system will try to defend the jaw, teeth, and muscles from
injury. A common abnormality is a gearing problem between
the teeth and the temporomandibular joint. If a gearing problem
exists, then the neuromuscular system programs reflex movements
for the lower jaw to help minimize damage to the teeth, their
supporting structures, and the temporomandibular joint. This
creates a situation in which the jaw is "limping,"
much as we limp with an injured ankle.
REBELLION
If life were perfect, the jaw could go merrily
along protecting itself. All the other muscles would adjust
and compensate for the compensation already being made by
the muscles of mastication. This is the way it usually happens.
Most people are able to get along quite well. But unfortunately,
muscles can sometimes be unforgiving of being pushed beyond
their normal physiologic limits for any length of time.
The most common way for a muscle to rebel is
to go into spasm—what we sometimes call a charley horse.
This condition is a painful contraction of the muscle. One
side effect of a muscle spasm is that it sends a message back
to the central nervous system. The central nervous system
then interprets this signal and causes the muscle in spasm
to contract even more.
Now the problem is more than the triggering
effect of a tooth-gearing problem. The spasm itself has caused
a problem: more painful contraction. When a muscle is in spasm,
its change in motion may affect other muscles. The muscle
spasm, through the central nervous system, creates more contraction,
which then creates more spasm, and this cycle goes on and
on. Because the muscles of mastication co-ordinate muscles
of the back and front of the body, any changes in these muscles
can result in postural problems and spasms elsewhere.
Now that you understand how the body supports,
balances, and protects itself, it's easy to see the cause
of some of the symptoms of TMJ. Because the muscles of mastication
are on the head, spasms in these muscles may result in headaches.
Pain can be, and often is, referred to other
areas. Referred pain is pain experienced in an area away from
the actual cause. Referred pain can be bizarre and may appear
to be unfounded.
If the muscle spasms happen to be in one of
the muscles that connect the skull to the spinal column and
shoulders, this may result in aching, stiffness, and restricted
movements in the neck and shoulders. Any muscle that is forced
to change its normal range of motion has the potential to
go into spasm. This is true of the entire chain. Thus, we
see back pain or stiffness in TMJ patients. We even see, although
rarely, TMJ symptoms exhibited in the hamstring muscles and
in the calves.
Muscle pain may make sense. But why, you ask,
would some patients with TMJ have symptoms such as ringing
or buzzing in the ears, earaches, dizziness, or even altered
hearing? A little muscle called Tensor veli palatini is responsible.
This muscle has many duties, one of which is to close off
the eustachian tubes. The eustachian tubes connect the throat
to the middle ear and are responsible for making air pressure
in the closed chamber of the middle ear equal to air pressure
outside. This occurrence is rarely noticeable. You probably
do notice your eustachian tubes at work when you clear your
ears during an elevator ride or in flight.
The Tensor veli palatini muscle gets its signal
from a branch of the same nerve that supplies the external
pterygoid muscle, one of the chief muscles involved in TMJ.
When the external pterygoid muscle goes into spasm, the Tensor
veli palatini also can contract because of the spasm/ contraction
feedback mechanism. Hence, with closed eustachian tubes, and
an inability to equalize middle-ear pressure, a patient can
experience symptoms that mimic middle-ear problems.
Another frequently reported symptom is numbness
in the hands and feet. There is a logical, if a bit complicated,
reason for this. The spinal column encloses the spinal cord,
which is the main nerve network connecting the brain to the
rest of the body. Nerves move from inside the spinal column
to the outside by passing through openings between the bones
of the spinal column. Because of the interweaving of muscles
between the bones of the spinal column, the nerves must pass
between layers of muscles. If these muscles are in spasm,
they may squeeze the nerves as they travel from the cord to
the fingers or toes. This can create numbness, which can be
mistaken for symptoms of neurological problems.
TMJ is basically a muscle-spasm problem. Because
of this, standard diagnostic tests, blood work- ups, EEGs,
or X-rays yield no information for a correct diagnosis. Often
a sufferer is led to believe that little can be done for the
problem except to block the pain rather than attacking the
reason for it. Sometimes a label is put on the headache—
migraine is a common one—not as a true diagnosis, but
in an effort to calm the patient. In many cases, attempts
to relieve the pain are in vain, leaving the TMJ patient suffering
and often feeling helpless.
THE PROBLEM AND THE SYMPTOMS
Although some people with tooth-gearing problems
have muscle spasms, others with the same problems don't. Why
are some patients with a tooth-gearing problem symptomatic
and others not? Why do people with symptoms experience them
with such varying severity and frequency?
We don't know why some people are susceptible
to muscle spasms; this is still a medical mystery. We can
only observe that some people appear to be more susceptible
than others. This is the same kind of mystery as why some
people rarely have infections or colds, and others exposed
to the same environment are constantly sick. Some people seem
to be constitutionally stronger than others.
Susceptibility, pain, and the pain threshold concept can't
be separated when discussing muscle spasms and their accompanying
symptoms. When a person's threshold to pain is high, a muscle
spasm may occur without pain. A person becomes symptomatic
when either the spasm becomes worse or the patient's pain
threshold drops. Sometimes both of these things happen.
It's still a mystery why a person's threshold
to pain changes, although stress is sometimes given as a cause.
We also don't know at what point a patient will experience
pain with a muscle spasm.
However, the degree of the muscle spasm will
go up and down in the course of the day in response to varying
stress levels. At a certain point, a spasm will be felt as
pain. The threshold level is the point at which the person
experiences pain.
We know that a person's threshold to stimuli
tends to increase as the stimuli remain. If we cut ourselves,
we may feel no pain at first and then experience intense pain
when we begin tending to the cut. But, as we know from experiencing
this kind of injury, the pain usually drops to a tolerable
level after a short time.
With TMJ problems that become symptomatic, we
don't know for sure if stress necessarily lowers the threshold
or increases the spasm. Perhaps both of these things happen.
But because the level of spasms and threshold change constantly,
people sometimes have intermittent symptoms: bouts with neck
and shoulder aches on stressful days, headaches at five in
the afternoon every day, more severe symptoms when the body
is stressed by unrelated illness, or headaches when especially
tired.
When people have mild headaches, for example,
and take an over-the-counter pain reliever, the central nervous
system's response to the pain stimulus changes. In effect,
when the pain reliever works, the person no longer feels the
pain because his or her threshold has been raised. However,
with TMJ patients, when symptoms are severe, neither over-the-counter
medications nor prescription drugs are effective in raising
the patient's threshold to the pain stimulus caused by the
muscle spasms.
HELP AVAILABLE
Much can be done to correct the source of the
muscle spasm and eliminate symptoms. But treating TMJ symptoms
can't even begin until the problem is diagnosed. Treatment
for TMJ depends on an accurate diagnosis of the condition.
Fortunately, as described in the next chapter, diagnostic
techniques are available.
|